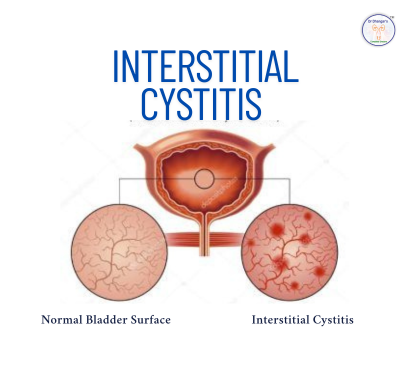
Interstitial cystitis (IC), also called bladder pain syndrome (BPS), is a chronic condition characterized by pelvic discomfort, urinary urgency, frequency, and pain, significantly affecting daily life Urologists address it with stepped care: dietary/lifestyle changes, oral medications, bladder instillations, physical therapy, and advanced interventions when necessary. Around 80% of patients respond to early-stage treatments over long-term .
2. Diagnosing IC/BPS
- Review of urinary symptoms & bladder diaries
- Urine analysis and cystoscopy with hydrodistension to assess bladder capacity or identify lesions
- Rule out other conditions like infection or stones
3. Step 1: Diet & Lifestyle Changes
- Eliminate triggers: caffeine, alcohol, citrus, spicy foods, artificial sweeteners
- Stay hydrated: dilute urine and reduce bladder irritation
- Bladder retraining: gradually increase voiding intervals
- Stress reduction: yoga, mindfulness and CBT can ease symptoms
- Symptom tracking: bladder diaries to identify personal dietary triggers
These measures alone often offer significant relief.
4. Step 2: Oral Medications
Commonly prescribed:
- Pentosan polysulfate (Elmiron) to rebuild the bladder lining
- Antihistamines like hydroxyzine for allergic-type bladder swelling
- Tricyclic antidepressants (e.g. amitriptyline) for pain and bladder spasms
- Pain relievers (NSAIDs) during flare-ups
Most urologists combine these sildenafil with diet and bladder training for best results.
5. Step 3: Bladder Instillation Therapy
Targeted delivery of medication directly into the bladder via catheter, allowing better absorption and relief without systemic side-effects . Medications used include:
- Lidocaine + steroids + heparin — calms pain and inflammation
- DMSO, hyaluronic acid if needed
Instillations are usually weekly sessions until symptoms improve.
6. Step 4: Pelvic Floor Physical Therapy
Many sufferers have tight pelvic muscles. Certified therapists:
- Identify trigger points
- Apply release techniques, biofeedback
- Teach exercises to relax pelvic floor
- Address posture and bladder coordination
Often used alongside oral meds or instillations.
7. Step 5: Advanced Options
For persistent cases even after prior treatments:
- Hydrodistension + cystoscopy to stretch bladder under anesthesia and detect lesions
- Fulguration/resction of Hunner’s lesions—special bladder ulcer type—during optimal cystoscopy
- Neuromodulation: TENS, sacral/tibial nerve stimulation for pain control
- Botox injections into bladder muscle—limited evidence but used in select cases
- Surgery (last resort): augmentation cystoplasty, diversion, or cystectomy used only for severe, refractory cases
8. long‑term Outlook
- 80% of patients have notable improvement with staged therapy
- Ongoing lifestyle management is vital to prevent flares
- Re‑evaluation (repeat cystoscopy or check for Hunner’s lesions) advised for non-responders
- Surgical outcomes are variable; used cautiously
9. Self‑Care & Living Well
- Carry flare‑management kit: meds, heat pad
- Avoid bladder irritants like caffeine, artificial sweeteners, alcohol, spicy foods
- Stay well hydrated, avoid dehydration
- Practice stress‑relief techniques
- Continue pelvic floor exercises
- Maintain follow‑ups for therapy adjustments
Interstitial cystitis is challenging but manageable. A stepwise approach—beginning with diet, hydration, bladder retraining, and medication—helps most individuals. Physical therapy and instillations enhance symptom control, while advanced neuromodulation or surgery are last resort options. With dedicated care and a trusted urologist, many regain a comfortable, active life.
FAQs
Q1. Is IC/BPS curable?
Although there is no definitive cure, most patients achieve symptom control and improved quality of life with staged therapies and lifestyle adjustments .
Q2. Are bladder instillations safe?
Yes—these deliver medication directly to the bladder with minimal systemic side effects. Mild discomfort or urgency immediately after is possible but temporary .
Q3. When is surgery considered?
Surgery (e.g., lesion removal, bladder augmentation) is reserved for those with severe, unresponsive disease—particularly those with identifiable Hunner’s lesions or low bladder capacity after all other options are exhausted .